
Chronic exertional compartment syndrome is one of the most common causes of pain, numbness, and foot drop, most often seen in runners.
The Tenex procedure is a non-surgical procedure that helps patients who are suffering from chronic tendon pain by removing damaged scar tissue on the tendons. This procedure, developed by Tenex Health, is particularly effective on the tendons of the shoulder, elbow, hip, knee, and ankle injuries. Conditions treated include tennis elbow/golfers elbow, rotator cuff tendonitis, Patellar tendonitis (jumper’s knee), Achilles tendonitis, and Plantar fascitis.
Tendon pain is typically caused by repetitive strain injury of sports and exercise. The Tenex procedure is known in medical terminology as focused aspiration of scar tissue, percutaneous tenotomy, and percutaneous fasciotomy. This is medical jargon for use a needle to remove the damaged portion of the tendon while preserving the rest of the tendon.
Ideal candidates have sought prior treatment, including injections, rest, immobilization, and physical therapy with no pain relief. The Tenex procedure offers patients a non-surgical option that is faster than traditional surgeries, creates a smaller incision resulting in less scarring, and allows for a quicker and less painful recovery.
Click here to learn more about Tenex!
The tendon scraping procedure is a successful treatment for chronic painful Achilles or Patella Tendonitis.
What is the procedure like?
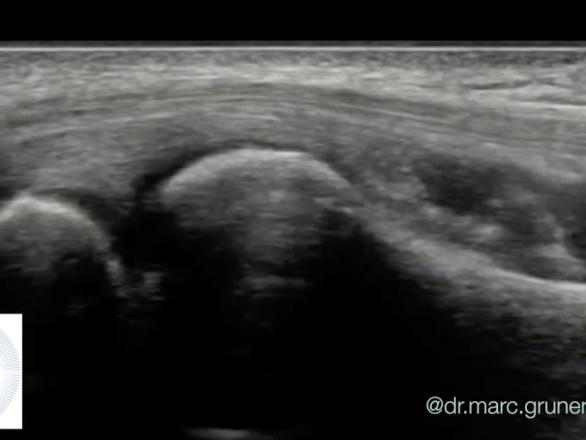
It is a minimally-invasive procedure performed under local anesthesia through a 2 mm long skin incision. The deep side of the tendon is visualized and the fat, blood vessels and nerves which cause pain and prevent the tendon from gliding well are scraped away from the deep side of the tendon. Scraping is guided by findings on ultrasound.
How long does it take to recover?
The procedure takes one hour and since the procedure is performed outside the tendon, the rehabilitation protocol is faster than other tendon procedures. Most patients can return to sport within 2-4 weeks.
This condition occurs when one of the major nerves in the hand is compressed as it travels through the wrist. The median nerve controls movement in the thumb and feeling in the thumb and first three fingers. The nerve runs through the wrist into the hand and can be entrapped by a tight ligament.
The non-surgical management of mild carpal tunnel syndrome can be accomplished with direct home care, which may include specific exercises, stretching, avoiding activities that cause symptoms, or wearing a wrist splint. Medications or corticosteroid injections may also be recommended.
What if surgery is an option?
More severe cases of CTS may be treated surgically through carpal tunnel
release (CTR), which involves cutting the transverse carpal ligament to relieve pressure on the median nerve. Traditional CTR procedures can remedy the condition, but may result in large and sometimes painful scars, prolonged pain, and a long road to recovery.
Sonex Carpal Tunnel Release
Carpal Tunnel Release (CTR) with the SX-One MicroKnife® and ultrasound guidance is a new and innovative surgical option for patients with severe carpal tunnel syndrome. CTR using ultrasound guidance relieves the symptoms of carpal tunnel syndrome while minimizing recovery time. Following the procedure, most patients can enjoy immediate motion and can return to work and the activities they love in 3-6 days.
Click here to learn more about Sonex!
Chronic exertional compartment syndrome is an exercise-induced muscle and nerve condition that causes leg pain, swelling and weakness. Anyone can develop the condition, but it’s more common in young adult runners and athletes. Chronic exertional compartment syndrome may respond to nonoperative treatment and activity modification. If nonoperative treatment doesn’t help, your doctor might recommend surgery.
Previous Treatment
Conventionally, treatment of compartment syndrome is open surgical fasciotomy to reduce pressure on the soft tissues. Surgical complications have included pain, scarring, adhesions, and infection. To reduce complications, less-invasive approaches have been developed in an effort to reduce postoperative pain, improve patient satisfaction, and reduce recovery time compared to surgery.
New Treatment
A novel treatment, consists of an incision 1/12 the size of previous incisions. The procedure is performed under ultrasound guidance and takes an hour to be performed. It is performed in the outpatient setting with no general anesthesia. Most patients are extremely satisfied, experience fewer complications compared to surgery, and are back to running in 10 days. Learn more about this treatment!
Trigger finger is a common condition in patients who do repetitive gripping or flexing of their fingers and hand. The tendons that flex the fingers run under a ligament, the A1 pulley, which keeps the tendons in place. In some cases, the tendons can get swollen from inflammation and develop a nodule that starts catching and popping under the ligament. In severe cases, the tendon can get so swollen that it will get stuck and will no longer bend the finger.
Frequently, the patient is offered a course of hand therapy to try to restore the full range of motion of the finger. In addition, anti-inflammatory medications, steroid injection, and a finger splint may be offered to treat the pain and inflammation.
For many years, the definitive treatment was surgery through an open incision, releasing the A1 pulley, and allowing it to heal in a stretched position. This would take the pressure off the finger, allowing the finger to bend again without getting stuck. However, an open release requires wound care, removing stitches a week after the procedure, risk of infection, and prolonged return to work due to the wound healing, and up to 4 weeks of restricted hand function. There is also potential for complications from the surgical healing, including pain and extensive scarring.
Currently, there is a minimally invasive technique to perform a similar release without a surgical incision. It is called a Percutaneous Trigger Finger Release Under Ultrasound Guidance. This procedure consists of injecting lidocaine locally to numb the area and releasing the A1 pulley with a needle under live ultrasound imaging. There is no incision with a scalpel so the recovery is much quicker, and with a much lower risk of infection. The patient can immediately bend the finger after the procedure, and the needle puncture can be managed with a band aid for 24 hours, without the need for stitches. In 3 days, the patient can resume light gripping, and can return to full gripping as soon as ten days. Pain and scar tissue formation are minimal given the lack of an incision. In addition, this procedure is cheaper than open surgery since it is performed in the office and does not require surgical fees.
What is it?
Frozen shoulder, or adhesive capsulitis, is a condition that causes pain and restricted movement in the shoulder. The joint of the shoulder is held together by a joint capsule, which becomes thickened and results in a global restriction of shoulder movement. This manifests with shoulder motion being stuck or frozen in all planes of motion, with loss of mobility especially apparent in external rotation as an early sign.
What causes frozen shoulder?
Frozen shoulder is a poorly understood disease. Genetic and environmental factors likely play an important role.
What are the symptoms of frozen shoulder?
Frozen shoulder progresses in a predictable manner.
Click here to see how Capsular Distention works!
301.493.8884
Dr. Mark D. Klaiman, MD
Monday – Friday 8am – 5pm
301.244.9099
Dr. Haim S. Hechtman, DPT
Monday – Thursday 7am – 7pm
Friday 7am – 5pm,
Saturday 8am – 1pm
“When I learned that my two favorite practitioners—who gave me back a normal, pain-free life—were joining their practices I thought, what a winner…..”
– Jane Stanley

Chronic exertional compartment syndrome is one of the most common causes of pain, numbness, and foot drop, most often seen in runners.

Hip arthritis is one of the most common causes of groin pain in patients. To diagnose it, we can use ultrasound. Ultrasound
Tennis elbow is one of the most common causes of elbow pain. The condition is also sometimes referred to as lateral epicondylitis.
Starting and sticking with a rehabilitation regimen has its challenges during the pandemic. Here are some ways to continue to progress.
|
Point Performance Medicine is Excited to Announce the use of Scrambler Therapy for the Treatment of Chronic Nerve Pain |